Benjamin M BruckerAlice DrainRachael D Sussman
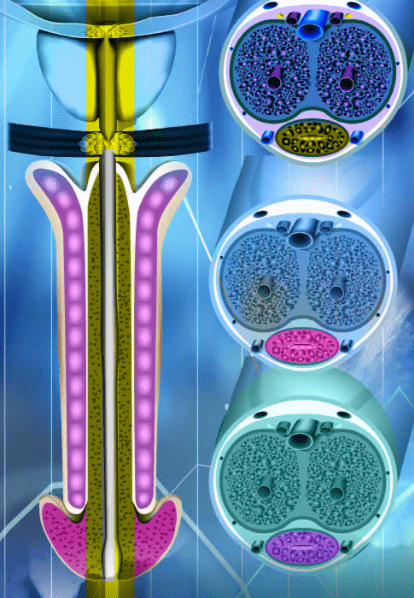
Primary bladder neck obstruction (PBNO) is a functional obstruction caused by abnormal opening of the bladder neck during the voiding phase of micturition. PBNO may present with a variety of symptoms including voiding symptoms (slow urinary stream, intermittent stream, incomplete emptying), storage symptoms (frequency, urgency, urgency incontinence, nocturia), and/or pelvic pain and discomfort. The diagnosis of PBNO can be made with videourodynamic testing, which demonstrates elevated voiding pressures with low flow, and fluoroscopic imaging demonstrating obstruction at the level of the bladder neck. Treatment options include conservative management with watchful waiting, pharmacologic management, and surgical intervention. In this article, we review the etiology, presentation, diagnosis, and treatment of PBNO in men, women, and children. [Rev Urol. 2019;21(2/3):53–62] © 2019 MedReviews®, LLC